-
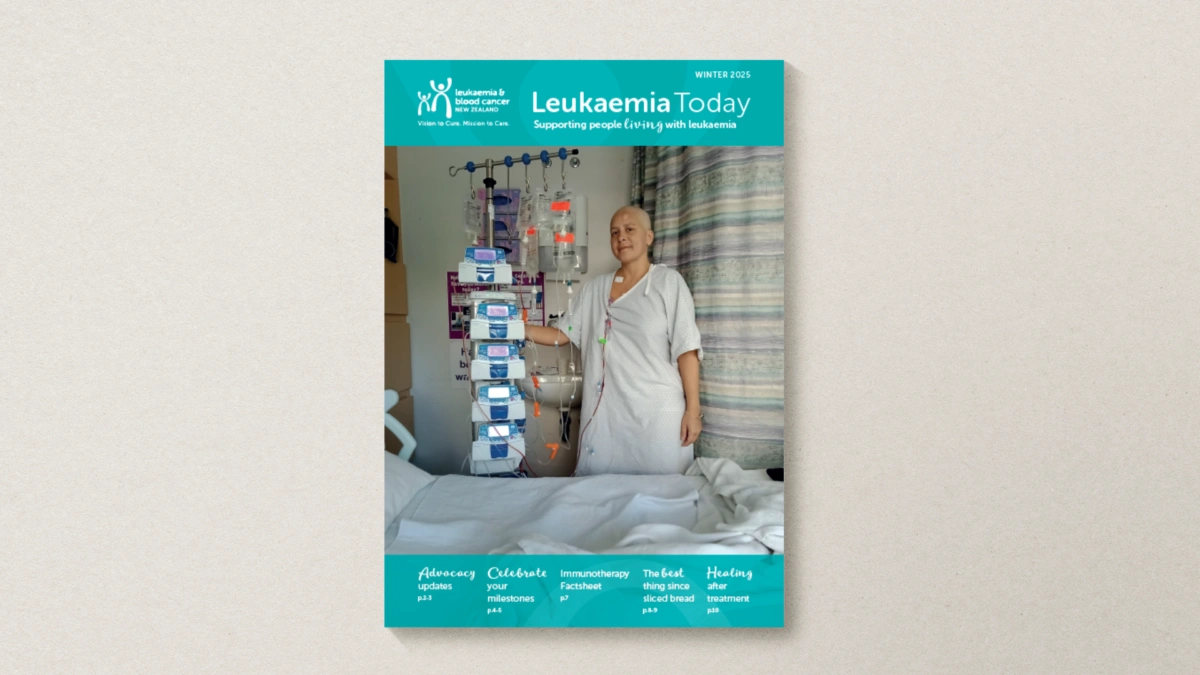 12 Jun 2025
12 Jun 2025Leukaemia Today | Winter 2025
-
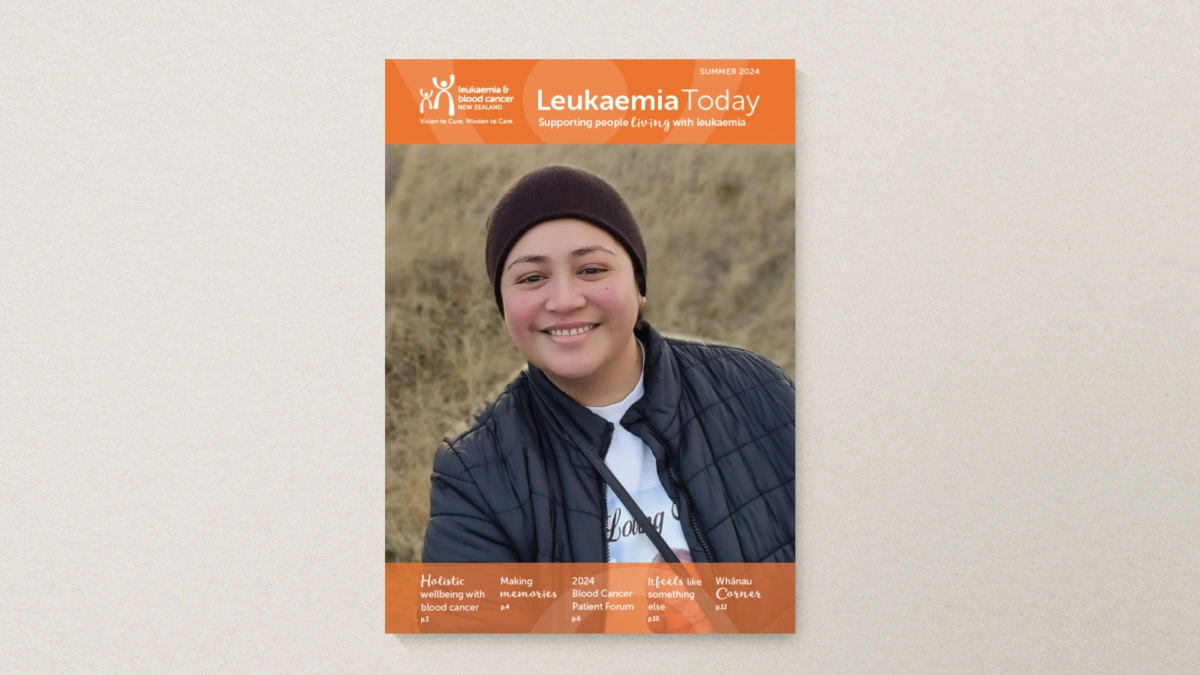 10 Dec 2024
10 Dec 2024Leukaemia Today | Summer 2024
-
 01 Jun 2024
01 Jun 2024Leukaemia Today | Winter 2024
-
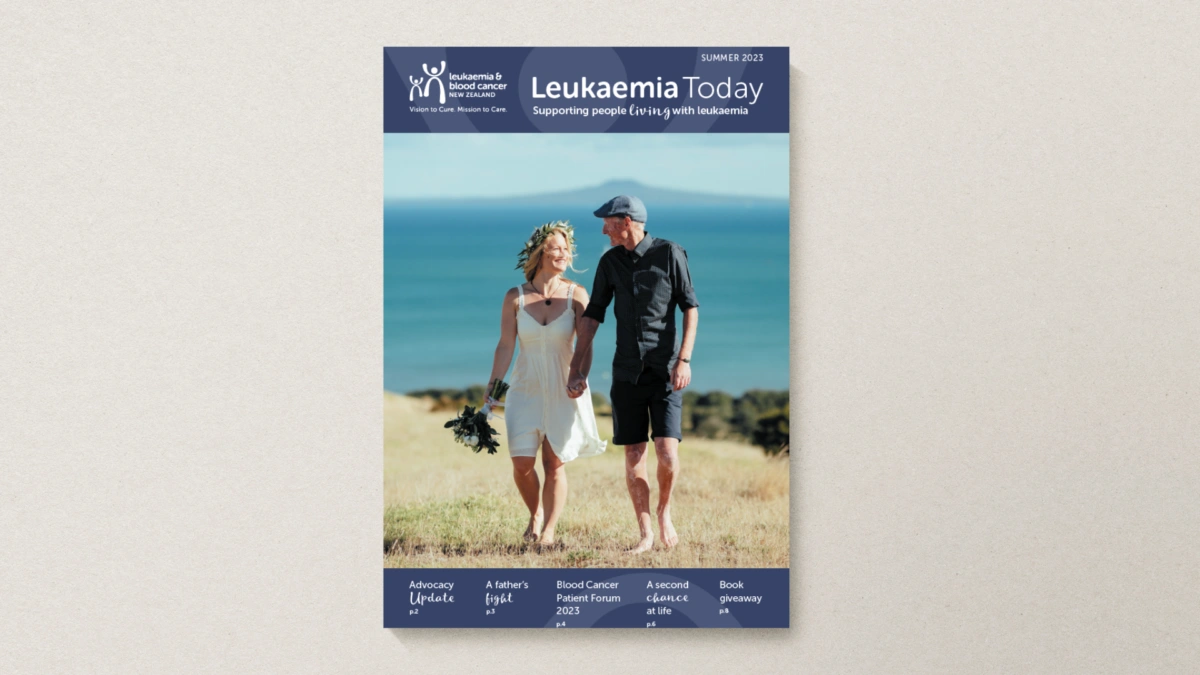 01 Dec 2023
01 Dec 2023Leukaemia Today | Summer 2023
-
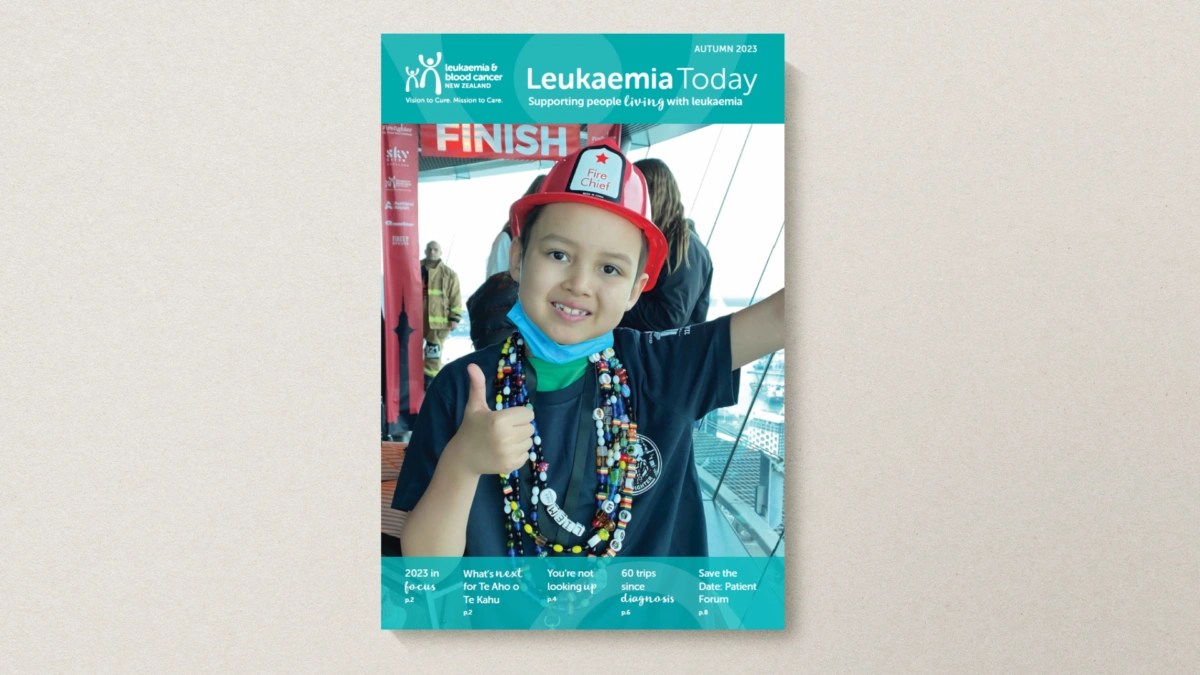 01 May 2023
01 May 2023Leukaemia Today | Autumn 2023
-
 01 Oct 2022
01 Oct 2022Leukaemia Today | Spring 2022
-
 01 Apr 2022
01 Apr 2022Leukaemia Today | Autumn 2022
-
 01 Aug 2021
01 Aug 2021Leukaemia Today | Winter 2021
-
 01 Nov 2020
01 Nov 2020Leukaemia Today | November 2020
-
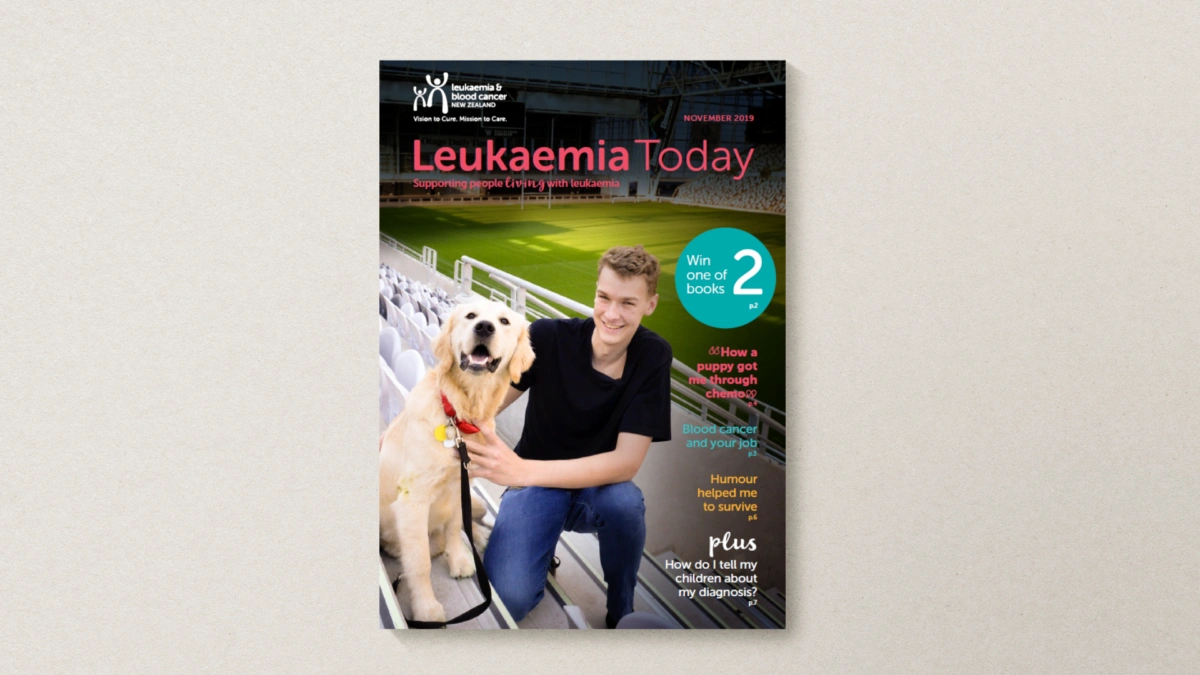 01 Nov 2019
01 Nov 2019Leukaemia Today | November 2019