-
 27 Aug 2024
27 Aug 2024Supporting life-saving cancer research
-
 27 Apr 2024
27 Apr 2024Innovation through research
-
 27 Jul 2022
27 Jul 2022Supporting future clinicians
-
 27 Nov 2021
27 Nov 2021Personalising medicine for blood cancer patients
-
 21 Sept 2021
21 Sept 2021New partnership to scale up CAR T-cell cancer treatment in New Zealand
-
 31 Mar 2021
31 Mar 2021Bringing cutting-edge treatment to Kiwis – a Vision to Cure
-
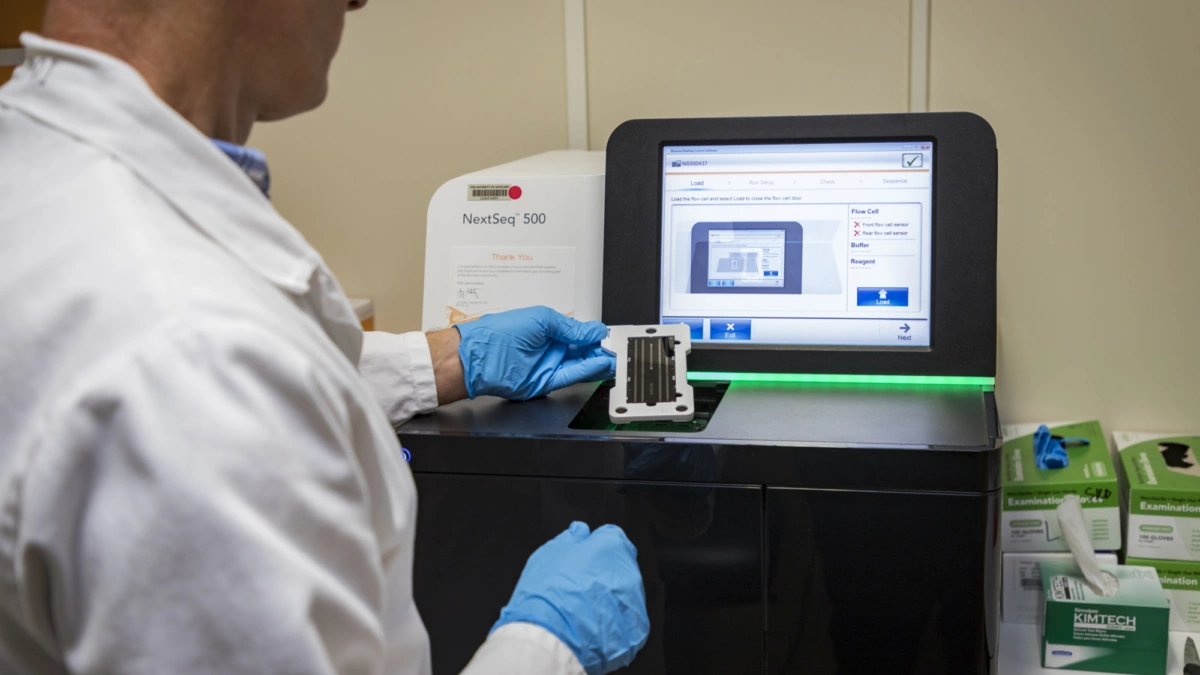
 27 Aug 2020
27 Aug 2020Gene sequencing – a Vision to Cure
-
 27 Jul 2019
27 Jul 2019UK’s drug-buying agency CEO: Why we like to say ‘yes’
-
 27 Jun 2019
27 Jun 2019Cancer Patients Miracle Means $540,000 Treatment Is Free
-
 07 Jun 2019
07 Jun 2019Do You Know About Haemochromatosis?